HILAR CHOLANGIOCARCINOMA (BILE DUCT CANCER)
Dr. Nikhil Agrawal | Last reviewed on
Bile duct cancer (cholangiocarcinoma)
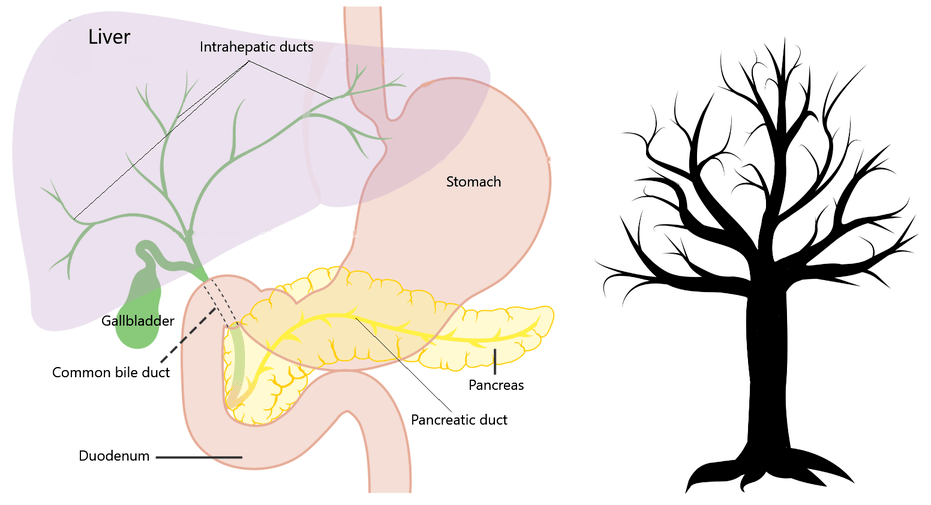
Cholangiocarcinoma is a cancer of the bile duct. In this, the inner lining of the bile duct (the tube that carries bile from the liver to intestine) becomes cancerous.
The bile duct is a network of thin tubes which originate in the liver like branches of a tree. The branches of the left and right side of the liver then combine to form two tubes called left and right duct, which then joins to form the common bile duct. The common bile duct joins the pancreatic duct at the ampulla of Vater and opens into part of the intestine called the duodenum.
The "joint" where the left and right bile duct join is called the "confluence or hilum". Hilar cholangiocarcinoma is a form of bile duct cancer which afflicts this part of the biliary tree. This is also termed perihilar cholangiocarcinoma or Klatskin tumour.
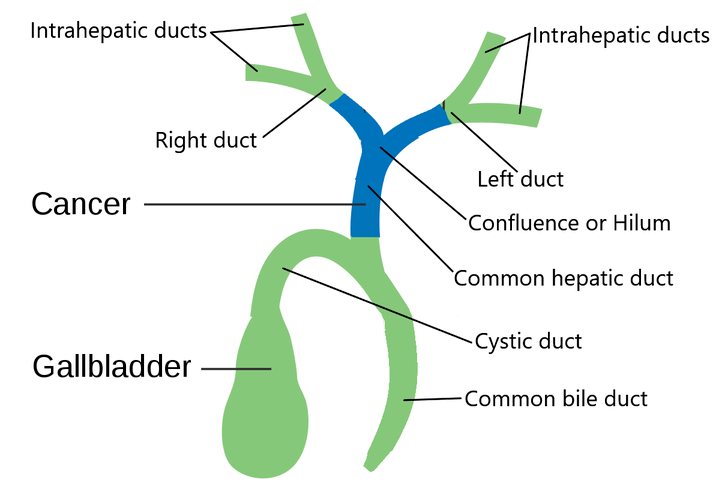
Hilar cholangiocarcinoma is the most common form of bile duct cancer and represents more than half of all cholangiocarcinomas.
When cancer affects the bile ducts which are still in the liver (intrahepatic ducts) it is called intrahepatic cholangiocarcinoma (bile duct cancer) . While cancer affecting the part of the duct where it joins the intestine is known as distal bile duct cancer .
Risk factors or causes of hilar cholangiocarcinoma
A risk factor is anything which increases the chance of someone getting a disease. Presence of a risk factor does not mean that the person will invariably get the disease, it only raises the probability of getting the disease.
Risk factors for hilar cholangiocarcinoma are:
- Old age
- Primary sclerosing cholangitis (PSC) - It is an autoimmune disease of the bile duct. In this persistent inflammation causes scarring and blockage of the ducts.
- Cysts of the bile duct (choledochal cysts and Carolis disease) - The lifetime incidence of cholangiocarcinoma in these patients ranges from 6% to 30%. The average age at malignancy detection is 32 years. The risk of malignancy decreases after excision of the cyst .
- Infection with liver flukes - Liver flukes are parasites that infest bile ducts and cause liver and bile duct diseases. The species causing disease in humans include Clonorchis, Opisthorchis and Fasciola.
- Cholelithiasis - In this condition stones form in the gallbladder. It is known to predispose to bile duct cancer.
- Cirrhosis - It is a late stage of scarring (fibrosis) of the liver caused by many forms of liver diseases.
- Viral hepatitis - Hepatitis B and C viruses cause a liver disease called hepatitis.
- Hepatolithiasis - It is a condition in which stones form in the bile duct within the liver. Cancer has been known to occur in 10% of such patients.
- Nonalcoholic fatty liver disease (NAFLD) and Nonalcoholic steatohepatitis (NASH) - These are diseases of the liver caused by obesity.
- Smoking and alcohol abuse
Signs and symptoms of hilar cholangiocarcinoma
Symptoms are our body's message to us that something is wrong. Cancer blocks the bile duct hindering the flow of bile from the intestine to the liver producing manifestations.
These symptoms include:
- Jaundice (yellowing of eyes, skin and urine)
- Itching
- Recurrent fever
- Unexplained weight loss
- Loss of appetite
- Pain abdomen (commonly in the right upper abdomen)
- Deranged liver function test
- Clay coloured stools
Diagnosis and staging of hilar cholangiocarcinoma
Hilar cholangiocarcinoma grows insidiously. Once a tumour is suspected, investigations are done to diagnose it and stage it.
These investigations include:
Blood tests: Includes routine blood tests, coagulation profile and liver function tests. It gives us information about the level of jaundice. Serum alkaline phosphatase and bilirubin levels are often elevated.
Tumour markers: These markers are substances in the blood which are measured and whose levels may be increased in the presence of cancer. CA19.9 and carcinoembryonic antigen (CEA) can be raised in cases of bile duct cancers.
Computed tomographic (CT) scan and magnetic resonance imaging (MRI): In CT the patient is scanned with a beam of x-rays, which is then computer-processed. MRI uses strong magnetic fields, radio waves and computer to generate the view of the inside of your body. While doing these investigations, intravenous contrast is injected into the blood circulation of the patient which enhances the images and delineates the blood vessels. Images are then acquired in phases (called triple-phase CT or MRI).
These studies give us the information about the extent of the disease, location of the tumour, how much it has spread in the bile duct, how much in the liver and its relation to the blood supply of the liver (hepatic artery, portal vein and their branches). It also provides information on the spread of disease into nearby or distant lymph nodes. Data is also obtained about the spread of the disease into the rest of the liver and abdominal cavity (distant spread of the disease).
Positron emission tomography (PET) scan: it is a functional imaging modality which is occasionally used as the hilar cholangiocarcinoma is usually not FDG avid.
Cholangiography: Endoscopic retrograde cholangiography (ERC) or percutaneous transhepatic cholangiography (PTC) provides excellent visualization of the biliary tree by injecting contrast into the biliary tree and taking images with the help of X-ray beams.
Biopsy or cytology: It is a procedure in which small bits of tissue or cells are obtained from the tumour by passing a needle under radiologic guidance. Cells can also be obtained by scraping with a brush while doing cholangiography (brush cytology). These are then examined under the microscope. A biopsy is usually not required if surgery can be done to remove the tumour. However, in locally advanced, unresectable or metastatic cancers, it is mandatory before starting further treatment. Because of fibrotic nature of these tumours obtaining a pathologic diagnosis sometimes becomes difficult. Endoscopic brushings and washings yield a positive result in only about 40%. A newer technique of fluorescent in situ hybridization (FISH) can enhance the accuracy of brush biopsies.
Staging of hilar cholangiocarcinoma
Staging tells us the current extent of the disease. The staging informs clinicians about the size of the tumour, its exact location, how much they have spread locally and whether they have spread to distant organs. It helps clinicians formulate a treatment plan.
The staging of hilar cholangiocarcinoma deepens on the extent of the tumour, extension into the bile duct on the right side and the left side and the relation of the tumour to the blood supply of liver (hepatic artery and portal vein and their right and left branches). Consideration is given to the amount of liver which will be required to remove the tumour and the remaining liver called functional liver remnant (FLR).
Bismuth and Corlette described criteria for categorizing these based on the extent to which the common hepatic duct, biliary confluence, and left and right ducts were involved by the tumour. This was further improved by researchers from Memorial Sloan-Kettering Cancer Center.
TNM (Tumour, Node and Metastasis) classification for staging
TNM (tumour, node and metastasis) classification developed by the American Joint Committee on Cancer (AJCC) is used for accurate classification of stage and it spans from I to IV. It depends on:
The extent (size) of the tumour (T): size and number of the tumour? Has cancer reached nearby structures or organs?
The spread to nearby lymph nodes (N): Has cancer spread to nearby lymph nodes? And to how many?
The spread (metastasis) to distant sites (M): Has cancer spread to distant lymph nodes or distant organs such as the peritoneum or lungs?
Treatment of hilar cholangiocarcinoma
The treatment of hilar cholangiocarcinoma depends on the stage at which it is detected. Surgical excision, when possible, is the best therapeutic option for hilar cholangiocarcinoma as it offers the possibility of a cure. In advanced stages, the treatment involves a procedure to decrease jaundice called PTBD, followed by chemotherapy, targeted therapy, immunotherapy, or radiotherapy.
Surgery for hilar cholangiocarcinoma: liver resection
The surgery for hilar cholangiocarcinoma is complicated by the fact that the liver tissue and blood supply of the liver (hepatic artery and portal vein and their branches) are in intimate relation to the bile duct. Besides a large part of the liver also needs to be removed.

The surgery for hilar cholangiocarcinoma involves removing the affected bile ducts within and outside the liver, including the confluence of the right and left hepatic ducts and the draining portal lymph nodes. Successful resection of the biliary confluence often requires removing the right liver, left liver or more, depending on the tumour size.
The surgical procedure to cut and remove a part of the liver is called hepatectomy or liver resection. Depending on the side and amount of liver resected these procedures are named right hepatectomy, left hepatectomy, extended right hepatectomy and extended left hepatectomy (right or left trisectionectomy).
The bile is directed to the intestine by connecting a loop of the small intestine to the cut end of the bile duct of the remaining liver. This procedure is known as hepaticojejunostomy.
Preoperative planning and workup
Patients are thoroughly assessed for fitness toward surgery. Their heart and lung are also checked. The amount of liver which is going to remain after surgery is carefully assessed for quality and volume.
Sometimes the amount of liver which needs to be removed is too large and hence the remaining liver is inadequate and not compatible with survival. In such cases, portal vein embolization can be done a few weeks before the surgery to increase the volume of the liver, which is going to remain after surgery.
If the jaundice is very high, then it needs to be brought down before the surgery by a procedure called percutaneous transhepatic biliary drainage (PTBD) or Endoscopic retrograde cholangiopancreatography (ERCP). In these procedures drainage tube is placed in the blocked bile duct, draining the bile and decreasing jaundice
After surgery chemotherapy or chemoradiotherapy may also be given in advanced cases to further improve the survival. This is called adjuvant treatment.
Liver transplant for hilar cholangiocarcinoma
In cases of locally advanced hilar cholangiocarcinoma that cannot be surgically removed and have not spread to other parts of the body, a liver transplant can be considered as a treatment option. Prior to the transplant, patients may undergo chemoradiotherapy.
Treatment – palliative
In cases where patients present with unresectable or metastatic disease, the primary objective of treatment is to provide palliative care, focusing on symptom management and improving the quality of life. Jaundice can be relieved through procedures such as percutaneous transhepatic biliary drainage (PTBD) and metallic stenting. Once jaundice is under control, chemotherapy or chemoradiotherapy is given. The aim is to extend survival and improve the overall quality of life for these patients.
Prognosis and survival
Many patients with hilar cholangiocarcinoma present in an advanced stage and are not in a condition to undergo surgery. Such patients have poor long term survival. However, in those who undergo surgery five-year survival rates following resection generally range from 25% to 50%.
Wish you a speedy recovery!


