Tumours and cysts of pancreas
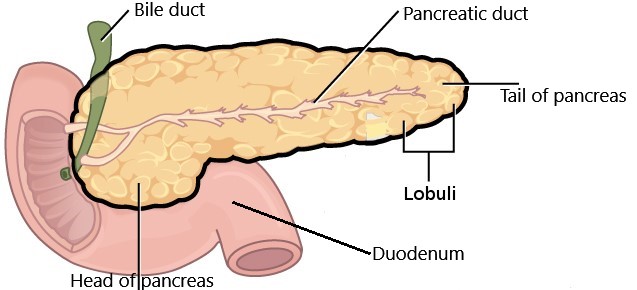
The pancreas is a flat soft organ in the upper abdomen behind your stomach. For description, it is divided into head, neck, body and tail. Blood supply of liver, intestine and spleen crosses perilously close to the pancreas. It is also intricately attached to the duodenum and bile duct.
The pancreas makes enzymes for digestion and various hormones, predominantly for control of sugar and metabolism.
Pancreatic lesions
Some cells in the pancreas may become cancerous, grows and then spreads, this is pancreatic cancer. Not only cancer but various other cystic and solid lesions afflict pancreas. Some of them are cancerous and some are benign (noncancerous).
These lesions include:
- Pancreatic pseudocyst
- Serous cystic neoplasm (cystadenoma)
- Mucinous cystic neoplasm (cystadenoma)
- Intraductal papillary mucinous neoplasm (IPMN)
- Neuroendocrine tumours
- Solid pseudopapillary neoplasm (tumour)
- Other rare tumours
Signs and symptoms
Majority of these cysts and tumours are small and do not announce themselves by causing symptoms. They are detected when ultrasound, CT or MRI is done to investigate unrelated symptoms. With advances in diagnostics, imaging and their frequent use, more and more such pancreatic lesions are being discovered.
When present the symptoms usually are:
- Pain abdomen
- Jaundice (yellowing of eyes, skin and urine)
- Feeling of fullness after food or bloating
- Lump in the abdomen
Diagnosis and investigations
Unfortunately, characterization of these is difficult, which means that distinguishing one lesion from another, and predicting cancer in them is arduous. This characterization nonetheless is required for formulating a treatment plan. So, more than one investigative modality is often required.
The commonly done investigations are
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
- Endoscopic ultrasound (EUS)
- Blood markers
Magnetic resonance imaging (MRI) is a modality in which strong magnetic fields, radio waves and the computer are used to generate images of the inside of your abdomen. This is the main investigative modality for pancreatic cystic lesions
Computed tomography (CT) is a diagnostic procedure in which the patient is scanned with a beam of x-rays. The resulting signals are computer-processed, generating slices of the image of inside. For better characterization intravenous contrast is administered and images are acquired in various phases of the passage of contrast through the pancreas, blood vessels and tumour (dual/triple phase).
Endoscopic ultrasound (EUS) is like doing an ultrasound of pancreas from inside of your stomach or duodenum with a special endoscope. Besides, tissue or fluid can be aspirated from the lesion, a procedure called fine needle aspiration cytology (FNAC) or biopsy (FNAB). It is examined under a microscope for the type of cells and various tests can be run on the fluid to ascertain the type of lesion.
Blood markers: Serum chromogranin and various hormones can be elevated in neuroendocrine tumours.
CYSTIC LESIONS
Pancreatic pseudocyst: This is the most common pancreatic cystic lesion. They are now called walled off pancreatic necrosis (WOPN/WON). These are sequelae of acute and chronic pancreatitis or trauma. It is a fluid-filled cavity lined with fibrous tissue. If symptomatic or infected they are treated with percutaneous drainage, endoscopic intervention or surgery. Surgery is now mostly done minimally invasively. It could either be cystogastrostomy or minimally invasive (laparoscopic or nephroscopic) pancreatic necrosectomy also called video assisted retroperitoneal debridement (VARD).
Serous cystic neoplasm (cystadenoma): These are more common in elderly females. It is composed of several small thin-walled spaces filled with serous fluid (microcystic appearance), frequently arranged around a central dense tissue. This lesion is usually considered benign (noncancerous) and has a low risk of becoming cancerous. Surgical excision is usually advocated in those with larger tumours (>4 cm) or inconclusive diagnosis.
Mucinous cystic neoplasm (cystadenoma): These cystic lesions of the pancreas have thick-walled cysts, which are usually larger than those of serous type and filled with mucin (macrocystic appearance). They are more frequently found in middle age women and the body and tail of the pancreas. Some of these lesions harbour cancer or may progress to cancer and hence surgical resection is done for some of these lesions.
Intraductal papillary mucinous neoplasm (IPMN): In this the lining of the pancreatic duct changes to mucin producing neoplastic cells which result in dilatation of the pancreatic duct. These more commonly occur in older individuals and the head of the pancreas. There are two types, main duct type and branch duct type. Chances of invasive cancer are more in main duct type IPMN and larger side branch IPMN and hence, these are usually operated. Asymptomatic and small side branch IPMN with features not suggestive of cancer can be observed with regular radiological follow-up.
Simple cysts and lymphoepithelial cysts are some other cysts which can occur in the pancreas. These usually do not require any treatment and are observed.
SOLID LESIONS
Pancreatic cancer: You can read about it here.
Neuroendocrine tumours: These are the most common solid pancreatic tumours after pancreatic cancer. They are brighter than other lesions in the arterial phase of the CT scan. Occasionally they can have cystic component also. They are more commonly found in the tail of the pancreas but can be located anywhere. Sometimes they secrete hormones and cause symptoms due to excess of that hormone. However, the majority are non-functional and do not secrete any hormone. Majority of these tumours are relatively slow-growing and cured by surgery. You can read more about it here.
Solid pseudopapillary neoplasm (tumour): It is a solid tumour with a cystic component. It predominantly occurs in young women. It grows slowly and causes symptoms when it is large enough. These generally do not turn cancerous and is cured by surgical removal.
Acinar cell carcinoma: It is a rare pancreatic tumour. If detected when it has not spread, it is treated with surgical excision of the tumour.
Pancreatic metastases: Metastasis is cancer which has spread from its original organ of origin to another organ, which is at a distance. Renal cell carcinoma (cancer of the kidney) and lung cancer are the most common tumours that metastasize to the pancreas.
Pancreatoblastoma, pancreatic lymphoma, focal pancreatitis, accessory intraparenchymal spleen are some other rare tumours.
Treatment
The treatment of these lesions depends on the type of lesion, symptoms and stage of the disease. For solid lesions generally, surgery is considered essential and is the gold standard. For some of the cystic lesions, decision making is quite complex and it is sometimes difficult to distinguish lesions that require surgery from lesions that do not require surgery.
Some of them, such as simple cyst, lymphoepithelial cysts, small serous cystic neoplasm, small branch duct IPMN and intraparenchymal spleen can be observed. They do not require surgical removal if they are not causing any symptoms. But there should not be any doubt in diagnosis if we decide to observe and they need to be diligently followed up to look for any changes in future, which might necessitate a change in plan.
However, the majority of the lesions will need surgical removal. The choice of surgical procedure depends on the location of the lesion in the pancreas. For tumours of the head of the pancreas, a Whipple procedure or pancreaticoduodenectomy is required. While for lesions in the body and tail of pancreas a laparoscopic or open distal pancreatectomy is done. Occasionally some lesions can be enucleated or removed by central pancreatectomy.
The prognosis depends on the type of tumour and the stage of the tumour. For the majority of them, long term prognosis is very good.
Wish you a speedy recovery!


