Rectal cancer
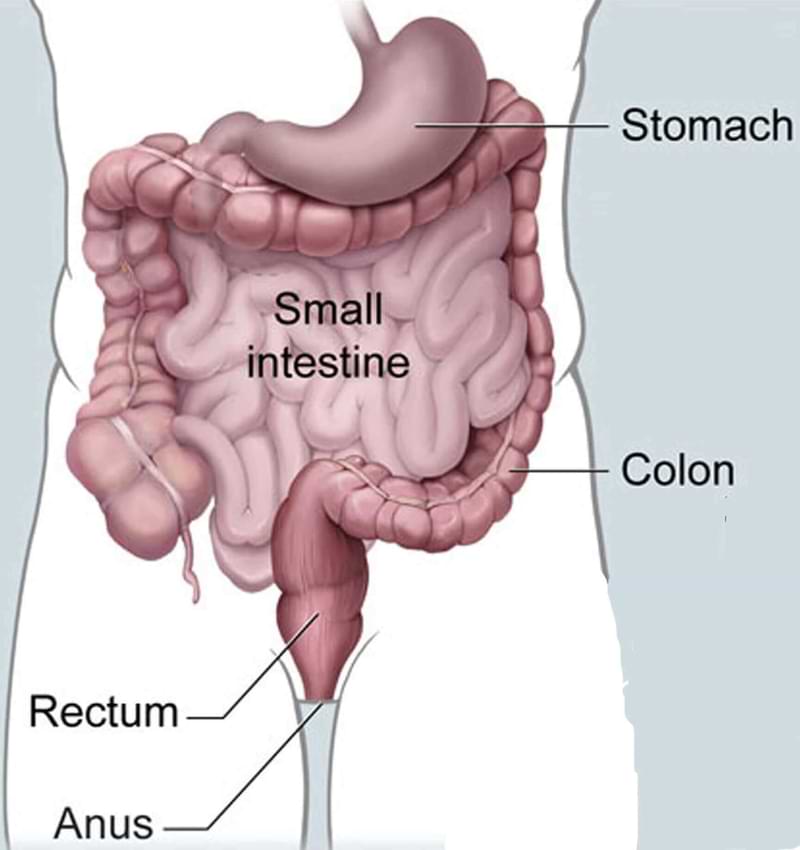
The rectum is the last part of the gastrointestinal tract. Rectal cancer and colon cancer are generally clubbed together and discussed as colorectal cancer. However, there are many important differences. Mainly because rectum sits in a narrow cavity called pelvis barely separated from adjacent orangs and bone. Moreover, many times the tumour is very close to the anal sphincter (the muscle ring responsible for holding the stools in the rectum). Because of these, the treatment of rectal cancer differs from colon cancer.
The rectal wall is made of four layers of tissue. Rectal cancer begins in the innermost layer, mucus-producing cells that line the rectum. Most of these start as a small mound of flesh called polyps. Over time some of these polyps develop into cancer which then advances and spreads. Rectal cancer is highly curable if detected early and treated appropriately.
Risk Factors for Rectal Cancer
Genetic
Some gene mutations run in families and increase the risk of colorectal cancer in that family. These, however, form a small proportion of patients with colorectal cancer.
The most common inherited colon cancer syndromes are:
-
Hereditary nonpolyposis colorectal cancer (HNPCC): HNPCC, also called Lynch syndrome, increases the risk of colon cancer and some other cancers. People with HNPCC tend to develop colorectal cancer before age 50.
-
Familial adenomatous polyposis (FAP): FAP is a rare disorder in which thousands of polyps develop in the lining of your colon and rectum. These polyps then turn into cancer. People with untreated FAP have a greatly increased risk of developing colorectal cancer before age 40.
Other risk factors
- Western diet (high fat and low fibre diet)
- Older age
- History of colorectal polyps
- Family history of colorectal cancer
- Inflammatory conditions of the colon, such as ulcerative colitis and Crohn's disease
- Diabetes and obesity
- Smoking and alcoholism
Diagnosis of Rectal Cancer
Diagnosis of colorectal cancer is established by doing a colonoscopy. It is a procedure in which a flexible thin tube with camera is passed and rectum is seen from inside. If any abnormality is seen then a small sample from it is obtained called as biopsy and examined under microscope confirming the diagnosis.
Symptoms of rectal cancer
These cancers like most other gastrointestinal cancers are asymptomatic in initial stages. The symptoms when occur would include:
- Change in bowel habits; persistent diarrhoea or constipation
- Feeling of incomplete evacuation
- Narrow stools or mucus in stool
- Painful bowel movements
- Unexplained fatigue and loss of appetite
- Unintentional weight loss
- Fall in haemoglobin (anemia)
- Pain or discomfort in abdomen
- Patches of dark blood in stool
Determining extent of disease (staging)
Depending upon the suspected extent of disease some of the following investigations will be done to determine the exact stage. In addition, various lab tests will be done to assess the function of other vital organs. Blood is also tested for CEA (carcinoembryonic antigen), which is produced by most colorectal cancers.
- Computed tomography (CT) scan
- Positron emission tomography (PET) scan
- Magnetic resonance imaging (MRI) scan
Following this work-up a stage will be assigned to the tumor, which spans from I to IV. It is based on three key elements.
The extent (size) of the tumor (T): How far has the cancer grown into the layers of the rectal wall? Has the cancer reached nearby structures or organs?
The spread to nearby lymph nodes (N): Has the cancer spread to nearby lymph nodes? And to how many?
The spread (metastasis) to distant sites (M): Has the cancer spread to distant lymph nodes or distant organs such as the liver or lungs?
Treatment of Rectal Cancer
Depending upon the stage and location of the tumour in the rectum, a treatment plan is made. Surgical resection is the mainstay of treatment in those with localized disease. In early tumours surgical resection is done first and then depending upon the final stage in biopsy report, chemotherapy or chemoradiotherapyis administered.
To obtain the best results for advanced tumours chemotherapy, radiotherapy and surgery are combined in an approach called multimodal treatment. Currently, the standard of care for advanced and low rectal cancers is the administration of chemotherapy or chemoradiotherapy first called neoadjuvant treatment, followed by surgery.
Chemotherapy is the use of special drugs to kill cancer cells and radiotherapy is the use of high-powered X-ray beams to kill cancer cells.
Surgery for rectal cancer
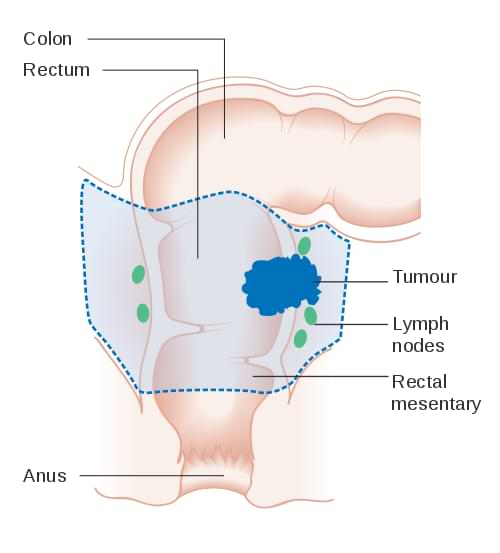
Treatment generally entails surgical removal of all of the cancer-bearing rectum with a margin of healthy tissue, along with adjacent lymph nodes. A piece of key information needed before surgery is how close the tumour is to the anus. If the cancer is infiltrating the anal canal then it is also excised. The surgical procedure to remove the whole or part of the rectum is given various names depending on the extent of colon and rectum resected. These names are anterior resection, low anterior resection, ultra-low anterior resection or abdominoperineal resection. The remaining ends of the colon and rectum are then reattached. If this attachment is not healthy or too close to the anal canal, then a diverting ileostomy is done, in which a loop of the small intestine is brought out onto the abdomen.
Sometimes the upper end of the colon is not reattached but brought out onto the abdomen by creating an opening in the wall of the abdomen. It is called a colostomy. This is required if the anal canal was also excised, a procedure called abdominoperineal resection. Another reason for doing this is when the operation is done for tumours completely blocking the lumen of the rectum. In both ileostomy and colostomy, the stool is collected into a bag that fits securely over the abdominal wall around opening.
Laparoscopic or Robotic surgery for rectal cancer
Rectal resection can be done in two ways; open and laparoscopic. In open surgery a single long incision is given over the abdomen and surgery is done. In laparoscopic approach the same surgery can be performed with minimally invasive techniques in which special surgical tools are inserted through small holes in the abdomen. This results in faster recovery and reduced pain compared to the conventional open surgery. This requires special expertise and make sure your surgeon is skilled and has done many of these operations.
Surgery for metastatic rectal cancer
Metastatic cancer is cancer that spreads from its site of origin to another part of the body. Metastatic GI cancers are generally considered incurable. Some stage IV cancers have spread limited to few spots of cancer in the lung, liver and peritoneum. If both rectal cancer and all these spots can be safely removed, then surgery can attempt to cure the disease.
Liver resection
It is a surgical procedure to remove cancer containing part of the liver, also called hepatectomy or metastasectomy.
Lung resection
Pulmonary (lung) resection is a surgical procedure to remove the part of the lung, which has cancer.
Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC)
Cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC) treats colorectal cancers that have limited spread to the abdominal cavity (peritoneum). During cytoreductive surgery, all visible tumours are surgically removed, which only leaves microscopic cancer cells. Cytoreductive surgery is followed by HIPEC, which aims to destroy the remaining microscopic cancer cells. In HIPEC, concentrated and heated chemotherapy solution is delivered directly into the abdominal cavity which kills those cells.
In these cases, we prefer to give chemotherapy first and then do the surgery. This approach helps the patients live longer and provides them with a chance to be free of cancer over the long term. We prefer to give neoadjuvant treatment before surgery in these patients.
Treatment of metastatic rectal cancer
If cancer has spread to a point where it cannot be completely removed by surgery, then it is considered incurable. Such cases are treated with chemotherapy. Chemotherapy prolongs life significantly. It also improves their quality of life.
Prognosis and survival
The metric to measure life after being diagnosis and treatment of cancer is 5-year survival. It tells you what percentage of people will be alive after five years. The exact number varies depending on the source of information. Survival after appropriate treatment depends upon the stage of the disease at presentation. After treatment for stage 1 colorectal cancer, the 5-year survival is slightly more than 90%. For stage 2 it is roughly 60–90%. The 5-year survival for stage III colorectal cancer varies from 45–90% and for stage 4, the 5-year survival is approximately 15%.

